All Baby Boomers should be screened for hepatitis C, according to federal recommendations. That’s because an estimated three-quarters of infections are in people born between 1945 and 1965, and most patients don’t know they’re infected.
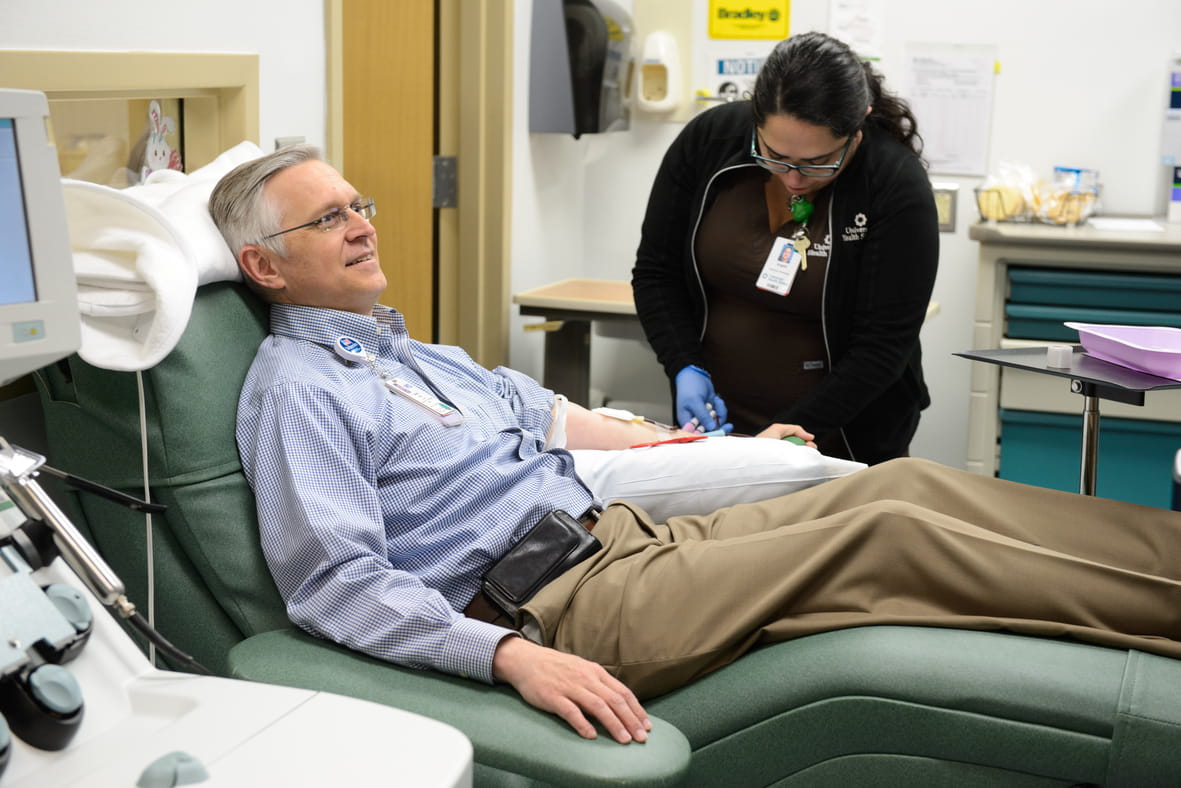
So far, most of that screening has taken place in clinics and doctors’ offices. But a newly published pilot study at University Hospital found that screening hospital patients for hepatitis C can catch many infections that outpatient testing misses.
“We tested about 95 percent of the people who’d never been screened before,” said Dr. Barbara Turner, an internal medicine physician and professor of medicine at the UT Health San Antonio, who led the study. “And of those, we followed up on over 90 percent with the (test for chronic infection) to see if they still had the infection. That’s remarkably high.”
Hepatitis C can cause cancer and liver failure
Hepatitis C is a viral infection that can lead to liver scarring and cancer. It’s a frequent reason for liver transplants. Although a percentage of patients clear the infection on their own, others develop chronic hepatitis C and can carry the infection for 20 years or more without symptoms, unaware they are infected. An estimated 2.7 million to 3.9 million Americans are thought to have chronic hepatitis C.
The study, funded by the Centers for Disease Control and Prevention, and published early online by the Journal of Hospital Medicine, identified 134 people with chronic hepatitis C infection out of more than 6,000 Baby Boomers admitted to University Hospital from December 2012 to January 2014.
Most were counseled and received follow-up primary care, with about 52 referred to a liver specialist.
The high cost of Hepatitis C treatments
Treatment proves a little more complicated, Dr. Turner said. A highly effective new class of hepatitis C drugs became available about halfway through the study. But with costs of close to $100,000 for a course of treatment, many uninsured patients rely on compassionate care discounts offered by drug companies to have access to them. Only a handful of patients in the pilot study have been approved, with applications from others pending.
And the costs for just screening and counseling those patients in the pilot project totaled $286,482, with little reimbursement to cover those costs.
“It’s a disease that even if you’re insured, it’s still a challenge normally with these marvelous drugs out there that cost $1,000 per pill,” Dr. Turner said.
How HIV programs could help
In the paper, the authors wrote that “it may be important for policymakers and payers to consider lessons from HIV programs. Because HIV-infected persons could not afford lifesaving medication, vigorous advocacy efforts led to legislation approving the Ryan White program in 1990 to fill gaps in HIV care that were not covered by other sources of support.”
Dr. Turner and her colleagues are now turning their attention to back to hepatitis C screening in outpatient sites, including University Health’s Robert B. Green Campus. They’ve received funds through the Texas 1115 Medicaid waiver and a grant from the Cancer Prevention and Research Institute of Texas to expand and improve screening in those outpatient settings.